Embolization Procedure:
Patient Assessment:
The first step is to evaluate overall health, coagulation status, and comorbidities in the medical history. With the help of imaging studies like CT angiography, MRI, or angiography precise anatomical mapping is done for comprehensive assessment.
The doctor explains the procedure, potential risks, benefits, and alternative treatments to the patient. Simultaneously, some blood test will be performed to evaluate coagulation parameters (PT, INR, aPTT) and complete blood count (CBC).
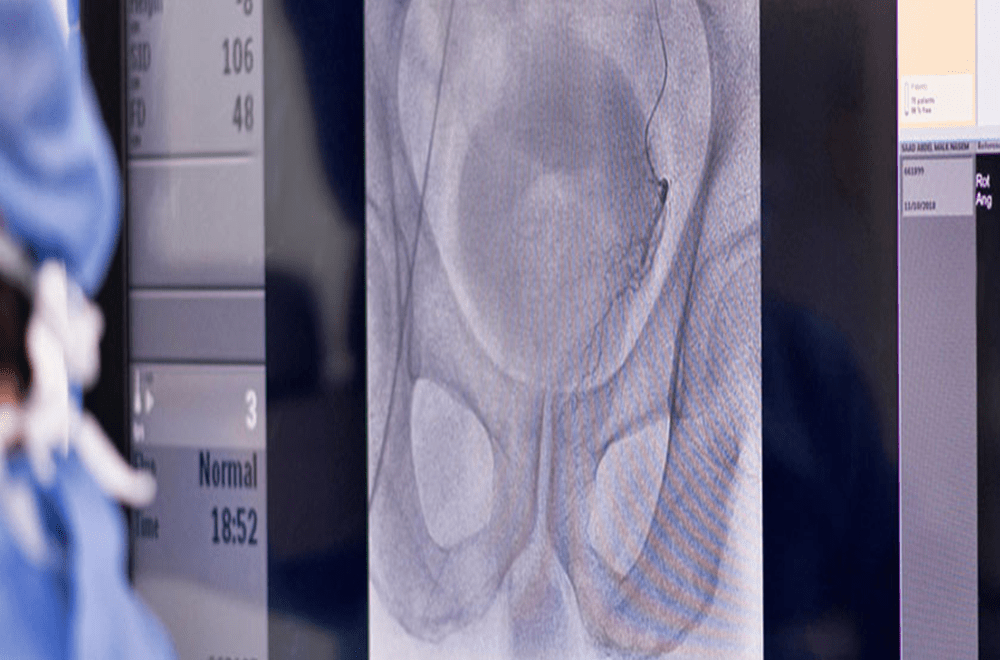
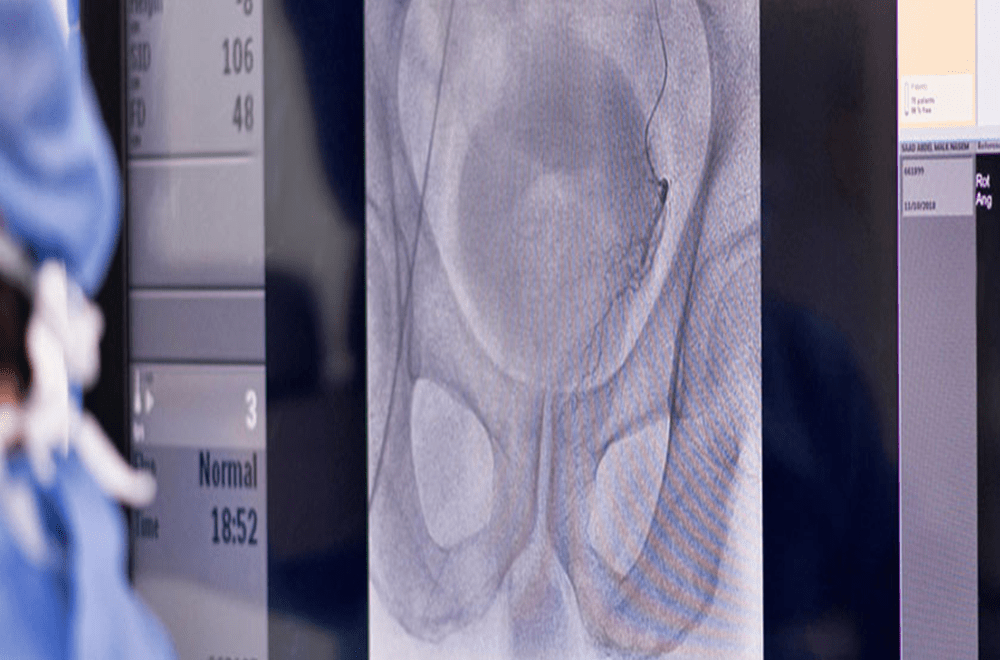
Procedural Steps:
The vascular access is usually through the femoral artery. Catheters are guided to the target vessels using fluoroscopic guidance.
Blood vessels are then visualized using contrast media to identify the target area.
The doctor places the catheter in a vessel that is supplying the target area and releases an embolic agent to obstruct blood flow.
Post-embolization imaging is then performed to confirm the success of the embolization and assess for any complications.
Post-procedural Care:
In the post-procedural phase, there is close monitoring of patients, checking of vital signs for stability, and prompt addressing of any pain. Complications such as ischemia and signs of infection at the access site are specifically noticed. If reperfusion occurs, re-intervene is swift. This will ensure the best outcomes for patients during this crucial period.
Follow-up:
Follow up comprises scheduled imaging studies to assess the effectiveness of the embolization over time.
Considerations:
Medical Indications:
Embolization is generally considered when other treatment options are not feasible or are less effective. Common applications include treating vascular malformations, stopping abnormal bleeding, and reducing blood supply to tumors.
Procedure Types:
Different embolization techniques exist, such as particle embolization, coil embolization, and liquid embolic agents. The choice depends on the specific condition being treated.
Pre-procedural Assessment:
Thorough patient evaluation and imaging studies are crucial to identify the location and nature of the vascular problem.
Recovery and Follow-up:
Post-procedural care and monitoring are important to ensure a successful outcome. Patients may need follow-up imaging to assess the effectiveness of the embolization.
Collaboration with Healthcare Team:
Collaboration among interventional radiologists, vascular surgeons, and other specialists is often required for comprehensive patient care.
Challenges:
Technical Expertise:
Performing embolization requires a high level of technical expertise. Interventional radiologists or specialists trained in vascular interventions typically conduct these procedures.
Patient Selection:
Identifying suitable candidates for embolization is crucial. Factors such as overall health, the specific condition being treated, and the patient’s anatomy play a role in decision-making.
Unintended Consequences:
There is a risk of unintended embolization, where the embolic material may travel to unintended areas, potentially causing harm.
Effectiveness:
The success of embolization varies depending on the condition being treated. Some conditions may require multiple procedures for optimal results.
Patient Compliance:
Patients may need to follow specific post-procedural instructions, and non-compliance can impact the success of the embolization.
Embolization benefits:
Embolization procedures offer a range of benefits in the management of various medical conditions. The specific advantages depend on the targeted pathology, but some common benefits include:
Non-Invasive Treatment:
Embolization is often a minimally invasive alternative to open surgery. It typically involves only a small incision for catheter placement, reducing the risks and complications associated with traditional surgical procedures.
Embolization procedure for fibroids saves the uterus and treats the disease too.
Selective Targeting:
Embolization allows for precise targeting of specific blood vessels. This selective approach minimizes damage to surrounding healthy tissues while addressing the pathology at its source.
Brain is a delicate area with very tiny vessels engulfed in its matter. Embolization procedure allows selective targeting and thus, minimizes the damage to the surrounding area.
Reduced Bleeding:
One of the primary applications of embolization is the control of bleeding. It can be highly effective in managing traumatic injuries, postpartum hemorrhage, or gastrointestinal bleeding by blocking the blood vessels that are the source of bleeding.
Tumor Treatment:
Embolization can be used as part of cancer treatment to reduce blood flow to tumors. This is beneficial for both preoperative tumor reduction and palliative care, where the goal is to alleviate symptoms associated with the tumor.
Varicocele Treatment:
Varicoceles, which are enlarged veins in the scrotum, can be treated through embolization. By blocking the abnormal blood flow, symptoms such as pain and infertility associated with varicoceles can be alleviated.
Minimized Hospital Stay:
In many cases, embolization procedures are performed on an outpatient basis or with a short hospital stay. This contributes to quicker recovery times and reduces healthcare costs.
Patients often experience shorter recovery times compared to traditional surgical interventions, allowing them to resume normal activities sooner.
Embolization side effects
While embolization procedures are generally considered safe and effective, like any medical intervention, they can be associated with certain side effects and potential complications. It’s important to note that the occurrence of side effects can vary depending on the specific procedure, the patient’s health, and the targeted condition. Here are some potential side effects and complications associated with embolization:
Pain or Discomfort:
Mild to moderate pain or discomfort at the catheter insertion site is common. This typically resolves within a short time.
Infection:
Infection at the catheter insertion site is a potential risk. Patients are typically prescribed antibiotics before the procedure to minimize this risk.
Allergic Reactions:
Rarely, patients may have an allergic reaction to the contrast dye used during angiography. This can cause symptoms such as rash, itching, or, in severe cases, anaphylaxis.
Ischemia:
The intentional blockage of blood vessels can lead to ischemia (lack of blood supply) in the targeted area. While this is often the desired effect, it can result in pain or tissue damage if not appropriately managed.
Blood Clots:
Embolization involves inducing clot formation. While this is intended in the targeted vessels, there is a potential risk of unintended clot formation elsewhere, leading to thromboembolic complications.
Post-Embolization Syndrome:
After certain embolization procedures, patients may experience a post-embolization syndrome characterized by fever, pain, and inflammation. This is usually temporary and can be managed with medications.
Infertility (Varicocele Embolization):
In the case of varicocele embolization, there is a risk of impaired sperm production, which may lead to temporary or permanent infertility.
Recurrence of Symptoms:
In some cases, the treated condition may reoccur, necessitating additional interventions or treatments.
With expert hands, these risks are further reduced. Dr. Imtiaz Ahmed is an accomplished interventional radiologist and endovascular surgeon with extensive experience in embolization procedures. His expertise lies in the non-invasive treatment of conditions such as fibroids, adenomyosis, uterine polyps, varicocele, and male infertility.
For more information email now at info@drimtiazahmad.com. Follow us on Instagram @Profdr_imtiaz_ahmad for daily updates.