OPD Timings
- Hameed Latif Hospital Lahore
Monday- Friday
(10 am to 8 pm)
Saturday
(12 pm to 8 pm)
Sunday OFF
- Omi Hospital
Monday to Friday
(9 am to 8 pm)
Saturday
(9 am to 8 pm)
Sunday OFF
Contact Info
- Karachi: (021) 32258075 – 79
Lahore: (042) 111 000 043 - Whatsapp: 03312597322
- info@drimtiazahmad.com
Ask the Experts
Genicular Artery Embolization

Overview
An 89-year-old man presented with several years of worsening pain in his right knee. Although he previously had no difficulty walking, at the time of presentation, he could only walk 3 blocks before stopping. Radiographs of the knee demonstrated severe osteoarthritis (OA) in the lateral compartment. The OA initially was managed with nonsteroidal anti-inflammatory medications and then with direct injections of glucocorticoids and hyaluronic acid. Joint injection resulted in only temporary relief. At that point, knee replacement surgery was recommended. Given his age, he was considered a moderate risk for general anesthesia complications. Moreover, he was concerned about a potentially lengthy recovery time. After seeking other treatment options, he chose to undergo geniculate artery embolization (GAE).
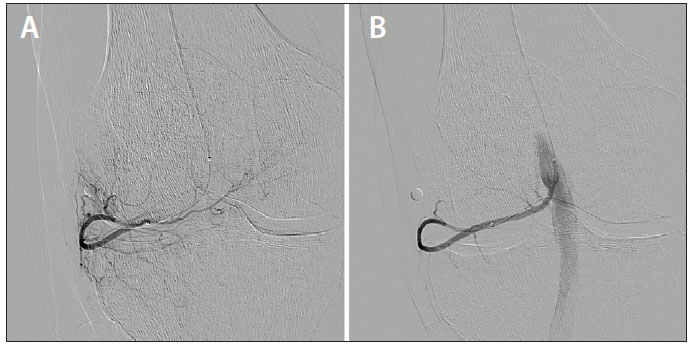
The procedure was performed with intravenous moderate sedation. A 3-F micropuncture sheath was inserted into the ipsilateral common femoral artery. Through the sheath, a 2.4-F microcatheter was used to select the popliteal artery. A small metallic object or “BB” was placed on the skin at the site of maximal pain. Angiography was performed and the lateral inferior genicular artery was catheterized. The angiograms demonstrated marked hyperemia at the exact location of the man’s pain. After embolization with 100-μm microspheres, the genicular artery remained patent and the hyperemia was resolved. The patient was discharged from the hospital 4 hours after removal of the catheter and manual pressure at the puncture site.
At 2 weeks after the procedure, the patient showed notable improvement in his pain and walked several blocks without difficulty. At 2 months, he hiked 3 miles without any difficulty. At 18 months, he continued to have sustained improvement in his symptoms.
Over the past decade, interventional radiology (IR) has witnessed a substantial transformation in our treatment armamentarium. Many interventional radiologists have trained in therapies that are now uncommonly performed today, but we have also cultivated numerous new minimally invasive treatments for diseases. Ablation and embolization are now the accepted and recommended treatments for liver cancer. Uterine artery embolization has a class A recommendation from the American College of Obstetricians and Gynecologists.1 Ablation for superficial venous disease has supplanted surgical vein stripping.
The development and adoption of these treatments share certain common elements. Each of these fulfilled a gap in the treatment algorithm where no adequate treatment existed. For example, prior to radioembolization, patients with hepatocellular carcinoma and portal vein thrombosis were referred to hospice. Hysterectomy was the only option for women with symptomatic multifibroid uterus after failure of medical management. People with symptomatic varicose veins had to either wear uncomfortable compression stockings or undergo a highly morbid vein-stripping surgery. In these instances, newer treatments did not necessarily compete with existing therapies; instead, they were a welcomed addition.
OA can be debilitating and can significantly impact an individual’s quality of life. Knee replacement surgery has a well-established track record, with excellent overall outcomes and a relatively low complication rate. However, many people are simply not ready to undergo knee replacement surgery, have concerns about the recovery time, have comorbid medical conditions that would place them at increased risk of complications, or are at a young age where they might need a knee replacement revision in 15 to 20 years.
For nonoperative intervention, localized injection of a steroid or hyaluronic acid has been the mainstay of treatment. However, the benefits of joint injection are temporary, necessitating repeat treatment. After repeated treatments, the effects diminish over time. Currently, no established therapy exists for those who have failed conservative therapy and are not good candidates for knee replacement surgery.
To succeed, GAE must find its appropriate place in the treatment algorithm. Similarly, adoption of this procedure should not be promoted with the promise of avoiding surgery entirely in all patients. As we have seen in uterine fibroid embolization, this threat can be met with hostility by our clinical colleagues, and it can conversely lead to obstacles in full adoption. Ideally, a multidisciplinary effort, as opposed to an adversarial approach, will result in more successful outcomes for patients.
In 2009, Zamboni and colleagues published results on angioplasty of the jugular and azygous veins for patients with multiple sclerosis (MS).2 Hailed as the “liberation procedure,” extracranial venous angioplasty was thought to have the potential to revolutionize treatment for MS. There was certainly a need for a new treatment because the available medical therapy was fraught with limited efficacy, significant toxicity, and high expense. The procedure itself was relatively straightforward, and initial single-arm trials yielded promising results. However, despite the initial enthusiasm for this treatment, venous angioplasty simply does not make sense from a pathophysiologic point of view. There is no reason to suspect that the symptoms in MS are caused by venous stenosis. Similarly, even if venous stenosis does occur due to MS, it is unclear how resolving it can alleviate symptoms. As a result, this was never widely accepted in the IR or neurology communities, and comparative trials eventually failed to show any benefit.3
Traditionally, OA has been thought of as a “wear-and-tear” disease. After years of cartilage and meniscal degeneration, physical contact between bones results in pain and disability. If it is simply due to wear and tear, embolization will not correct this pathology. Although traditional cellular inflammation (eg, increased leukocytes in the joint space) may not be present in OA, proinflammatory mediators at the molecular level are indeed secreted from the synovium, leading to joint tissue destruction.4 If embolization can decrease synovial inflammation and subsequently decrease the circulation of inflammatory cytokines, the viability of arterial embolization in alleviating symptoms and reducing the rate of joint degeneration may be validated.
Cross-sectional imaging traditionally has allowed us to prove that embolic therapies have an effect. For example, when objective response is achieved in contrast-enhanced imaging after hepatic artery embolization for hepatocellular carcinoma, it has been shown to result in a longer time to progression and longer overall survival. In contrast, we currently do not have an objective way to assess the active component of OA. Future studies will need to focus on detecting these inflammatory markers in the joint fluid before and after embolization to determine if embolization indeed reduces inflammation.
Today, the threshold for the medical community to accept a new minimally invasive therapy is extraordinarily high. A minimally invasive procedure such as embolization is always met with skepticism by our medical and surgical colleagues because it defies the conventional way of treating disease. As an example, radioembolization has shown survival of > 12 months in patients with tumor-associated portal vein thrombosis in multiple single-arm prospective trials. However, the medical oncology community has been reluctant to accept radioembolization in its treatment algorithms, citing a lack of comparative data. Yet, when immune checkpoint inhibitors demonstrate mildly promising rates of objective response in single-arm trials, a great deal of enthusiasm ensues.
For OA embolization to truly gain acceptance, prospective trials need to show safety and efficacy as well as (eventually) superiority to conventional treatments. Initially, single-arm trials must demonstrate the safety of GAE with regard to significant adverse events. Nontarget embolization, which could result in foot ischemia, nerve injury, skin necrosis, or osteonecrosis, is a primary concern. These complications must be avoided at all costs. Unlike patients with malignancy, where complications may be expected to occur, the adverse event rates for both joint injections and knee replacement surgery are low. Therefore, embolization must show that adverse events rates are similarly low.
If single-arm trials show acceptably low rates of adverse events and promising efficacy data, comparative trials will eventually be necessary. Pain and function are difficult to quantify and reproduce. Studies assessing pain and functionality often have a placebo effect, such as that seen in the angioplasty for MS trials. Standardized criteria, such as the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), exist to assess the degree of disability from OA. However, a placebo effect can even exist in the reduction of WOMAC scores. Interestingly, a comparative trial of hyaluronic acid injection versus placebo yielded similar improvements in pain and functionality.5 Ultimately, a comparative trial of GAE versus either placebo or standard of care will need to be done. There are multiple practical challenges in designing such a study; however, this has been successful for uterine fibroid embolization, which has been compared to hysterectomy in multiple well-designed studies.
OA is a multifactorial process, and there exists a wide range of OA severity. GAE may be clinically effective in certain degrees of OA, but it is very likely that it will not be effective in the entire range of severity. In the very early stage (ie, mild joint space narrowing) and very advanced stage (ie, complete cartilage and meniscus loss with bone-on-bone contact), GAE may play a significant role or none at all. When designing trials in the future and offering GAE, it will be imperative to select the appropriate patients. Simply offering GAE in the most advanced cases, where limited benefit is likely to be seen, may deter its adoption. For example, recent randomized trials for radioembolization versus systemic therapy failed to show a survival benefit for radioembolization, largely because a significant proportion of the patient population had advanced hepatocellular carcinoma beyond currently accepted radioembolization guidelines.6 Is it possible that the trial may have shown better efficacy in patients with slightly less advanced disease?
If GAE is shown to be effective in the treatment of knee OA, it will launch an entirely novel avenue for the practice of embolization. In the United States, over 600,000 people develop knee OA every year, with a relatively equal frequency between men and women.7 In comparison, approximately 42,000 people develop hepatocellular carcinoma every year in the United States.8 OA would potentially be the highest-prevalent disease that could be treated by a minimally invasive, image-guided procedure such as embolization.
Arterial embolization for OA can also expand outside the knee. Reports of embolization of the shoulder for adhesive capsulitis and the elbow for lateral epicondylitis have shown promising results.9,10 Other inflammatory disorders such as rheumatoid arthritis, for which treatment options are sorely needed, may be even more susceptible to embolization.
Over the next several years, we will determine whether arterial embolization is a viable treatment for OA. If not, like many other attempts in endovascular intervention, we will restart and continue to seek minimally invasive treatments for other conditions. If arterial embolization is determined to be a viable treatment, it will have a profound impact on IR.
- ACOG practice bulletin. Alternatives to hysterectomy in the management of leiomyomas. Obstet Gynecol. 2008;112:387-400.
- Zamboni P, Galeotti R, Menegatti E, et al. A prospective open-label study of endovascular treatment of chronic cerebrospinal venous insufficiency. J Vasc Surg. 2009;50:1348-1358.
- Zamboni P, Tesio L, Galimberti S, et al. Efficacy and safety of extracranial vein angioplasty in multiple sclerosis: a randomized clinical trial. JAMA Neurol. 2018;75:35-43.
- Bonnet CS, Walsh DA. Osteoarthritis, angiogenesis and inflammation. Rheumatology (Oxford). 2005;44:7-16.
- Jevsevar D, Donnelly P, Brown GA, Cummins DS. Viscosupplementation for osteoarthritis of the knee: a systematic review of the evidence. J Bone Joint Surg Am. 2015;97:2047-2060.
- Vilgrain V, Pereira H, Assenat E, et al. Efficacy and safety of selective internal radiotherapy with yttrium-90 resin microspheres compared with sorafenib in locally advanced and inoperable hepatocellular carcinoma (SARAH): an open-label randomised controlled phase 3 trial. Lancet Oncol. 2017;18:1624-1636.
- Zhang Y, Jordan JM. Epidemiology of osteoarthritis. Clin Geriatr Med. 2010;26:355-369.
- National Cancer Institute. Cancer stat facts: liver and intrahepatic bile duct cancer. https://seer.cancer.gov/statfacts/html/livibd.html. Accessed March 21, 2019.
- Okuno Y, Iwamoto W, Matsumura N, et al. Clinical outcomes of transcatheter arterial embolization for adhesive capsulitis resistant to conservative treatment. J Vasc Interv Radiol. 2017;28:161-167.
- Iwamoto W, Okuno Y, Matsumura N, et al. Transcatheter arterial embolization of abnormal vessels as a treatment for lateral epicondylitis refractory to conservative treatment: a pilot study with a 2-year follow-up. J Shoulder Elbow Surg. 2017;26:1335-1341.
Since the procedure is so new, some insurance companies may not offer coverage for PAE unless certain conditions are met, like having blood in the urine (hematuria). After discussing your medical history with you, we can check on coverage with your insurance company.
Yale Medicine’s commitment to multidisciplinary care is a true differentiator that ensures every man gets the optimal treatment for his condition. Because we have a multidisciplinary team of experts, you can have a urologist evaluate your BPH symptoms and discuss all your treatment options with you, including PAE. We are one of the few medical institutions in the country regularly performing this procedure for our patients.
Dr. Ahmad has been practicing in the health care industry for more than 20 years.
In 1995 he completed his fellowship at Northwestern University Chicago Illinois USA.
